I’ve been reading back through my posts as funnily enough- I have forgotten what I wrote! No surprise there with the state of my brain at the moment! A lot has been my slant on things so I thought I’d zoom in on some of the facts in case you’re looking for them here on my site. I am not a medically trained doctor (only a mere psychologically trained one!) but I’ve done a lot of reading and these are my conclusions based on the literature. I’d urge you to seek help from your GP to discuss any new or persistent changes that you’re worried about and do it sooner rather than later. That way you get ahead of the game. Never think you’re wasting the doctor’s time- that’s what they’re there for. Remember that you are the expert on your own health, so verbalise this, let them know what you’re thinking, what you’re experiencing, and let them know what you want, be it support, information, therapy or treatment.
Perimenopause means….
The term Perimenopause means before the menopause, and menopause is official once you’ve had no period for 12 months. The average age in the UK for menopause is 51, so if you’re in your 40s, the Perimenopause should very much be on your radar. The range of onset of menopause is 45-55 and the Perimenopause can last for a decade beforehand so you could start to see things change earlier than your 40s. Perimenopause often occurs during a busy time in women’s lives when they might have more responsibilities at work and home, so many women do not notice the changes start to creep in nor link them together.
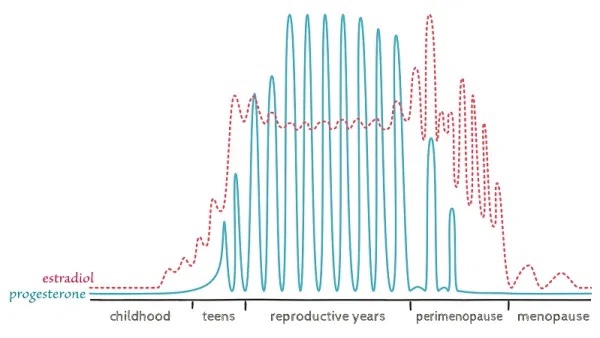
During the perimenopause, our key female hormones start to deplete. This does not follow a linear pattern, instead hormones fluctuate up and down in a gradual downwards pattern, until our ovaries stop producing oestrogen and we stop ovulating and this is perfectly normal. This fluctuation in both oestrogen and progesterone, is the reason why our periods change one month to the next during Perimenopause and why mood can be up and down, although it is not a direct correlation and hard to predict. Your GP is unlikely to do a blood test to check your hormones because of these frequent fluctuations, so the reading wouldn’t explain much. You may only be offered a blood test if you are under 45, if early menopause is suspected.
This can make it very hard to know what’s going on with your body and whether you are in Perimenopause. Please don’t discount Perimenopause if you are under 45 as you could well be experiencing changes around this time, as I did but I dismissed the signs and attributed them to other things for too long and I think this not knowing, heightened the distress. Below are some of the changes you might experience, but not all women experience all of these because we are humans, and therefore individuals with very different bodies, brains and vulnerabilities. Remember that these changes are temporary because the body and the brain recalibrates and adapts after menopause and things settle down.
PERIODS CHANGES
During Perimenopause, your periods start to change. They can become lighter and less frequent which is what I expected but for many women they become heavier and more frequent or all over the place. Passing clots is not uncommon as are flash periods i.e. random, sudden gushes of blood. This is due to an imbalance between progesterone and oestrogen, where oestrogen is high compared to progesterone, so the uterine lining grows, resulting in heavier bleeding when it sheds. Heavy periods are defined as soaking through a pad or tampon per hour, requiring double protection, disturbing your sleep, or lasting longer than 7 days. Heavy bleeding can lead to anaemia, exhaustion and fatigue. As this phase of the menopause can last several months or years it’s worth speaking to your GP about options for managing this, including birth control such as the mirena coil which can make periods lighter and more manageable.
Shorter cycles are common in early Perimenopause so it’s common to feel as though you’ve just finished your period and you’re starting again. Later in Perimenopause the cycle gets longer and more spaced apart. Longer cycles are defined as 38 days or more apart. These are linked to cycles in which anovulation occurs, in other words you’re not producing an egg at those times. Missed periods also occur at this stage. If your period does still eventually arrive, this means you are still ovulating and can still get pregnant. Eventually we know that periods do stop (hooray!) and menopause is diagnosed once you haven’t had a period for 12 months.
Post menopause, any spotting or bleeding should be assessed so go to see your GP.
BRAIN FOG
Perimenopause is a time of neurological change when our brains are influenced by hormonal fluctuations. Brain fog is the term used, but it encompasses any cognitive change including memory, attention, concentration, word finding difficulties, visual perceptual disturbances (resulting in clumsiness) and confusion. It’s thought that declining and fluctuating oestrogen in the hippocampus and frontal cortex is linked to cognitive changes at this time because oestrogen has a protective function in our brains. It’s thought that hot flushes during the night, disturbing sleep are closely linked to the extent of brain fog and so hormonal replacement can help to manage both of these symptoms. The benefits of HRT on brain fog are not clear cut but studies show that use of HRT early in Perimenopause shows the most benefits. The good news is, that thanks to the brain’s neuroplasticity, our post menopausal brain adapts and brain function returns to normal. So please don’t think that brain fog during Perimenopause determines or is linked to early onset dementia, as this is not the case.
MOOD
Mood changes like irritability, tearfulness, higher emotion sensitivity, plus the physical manifestations of anxiety (e.g. palpitations, sweating, stomach and chest discomfort) and cognitive aspects of anxiety (e.g. worry, self criticism, and overthinking) are very common during Perimenopause. As with all the other changes, not all women experience this and it can be different for each. This is due to the complex interaction between the change in hormones and each individual’s brain, plus their own history for example prior trauma or loss, personality and life circumstances. HRT can help some women with mood changes in Perimenopause and it’s important not to miss this and jump straight to antidepressants. If women have had mood changes in the past there is the risk that the role of the Perimenopause and hormones might be missed. Each episode of distress should be assessed on its own merits considering new and previous ways of managing and treatment. Identifying ways to reduce and manage stress, and finding support and time for yourself, while you work all this out, is very important. Lots of women lose their confidence and self esteem due to concerns about brain fog, feeling anxious or tearful, plus lack of sleep and hormonal changes that heighten emotional sensitivity. Normalising emotionality during perimenopause would have massively reduced my concerns about it, framing and contextualising it so that I didn’t wonder what was wrong. I’m sure it would have helped. This is why I’m passionate about sharing my experiences.
There will be a line in the sand, however where some women with mood changes will say they’re not coping and for whom HRT does not help. Where women have a background of trauma, loss or emotional sensitivity this can be a particularly difficult time. Similarly, survival strategies that you might have worked through and managed for a time might now pop up again for example eating difficulties, self harm, alcohol or substance misuse, obsessions or compulsions, isolating and withdrawing from people. This is where good assessment is vital when women present with mood changes during Perimenopause, because each woman will have different needs and will benefit from different interventions. It can be really helpful to see a psychologist who could help you to make sense of any mood changes that you are struggling with, whether this is new or recurring plus learn ways to manage this. It’s very important that any health professional working with you knows about a trauma background, as some treatment methods or approaches might inadvertently trigger PTSD symptoms. Technically any health professional should be trauma trained and informed but this sadly is not always the case so let them know. Read my Perimenopause and trauma blog for more. Women should be able to make informed choices around managing their mental health so whether they choose to try HRT, psychiatric meds like anti depressants or try therapy or lifestyle changes or any combination of these, this must been done safely and in line with the woman’s wishes and reviewed frequently. Keeping a biopsychosocial model at the forefront will ensure that recommendations and interventions are tailored carefully to each woman based on their history.
INFLAMMATION
Joint pain is common during Perimenopause, due to decreasing levels of oestrogen which has an anti inflammatory effect in the body. Skin itching or crawling can be felt and disturbs sleep. Dry and itchy eyes can occur. Stomach and bowel discomfort and UTIs can be bothersome. It’s always worth having any new symptoms assessed to be on the safe side. Perimenopause is a good time to look at nutrition as this can massively help with skin and stomach complaints, plus it’s important to make sure you’re putting all the good stuff in, like vitamins, minerals, protein and essential oils. This helps to keep our bodies strong and fight inflammation especially when our oestrogen levels are down. This in turn will help prevent against injury, boost heart health, muscle mass and brain health.
SLEEP
Trouble getting to sleep or wakening through the night or waking too early is common in Perimenopause. Sleep is so important for our health at all ages and underpins every single system in our body. It’s thought that when we sleep our body breaks down toxins, creates deep relaxation and during REM sleep, processes our day, filing away memories and discarding any unessential information from the day. So REM sleep is our therapist and much needed. Dr Maki has been studying hot flashes and the effect on cognition and she found that Perimenopausal women wearing a monitor whilst sleeping could experience many observable temperature fluctuations during the night that disturbed their sleep but the women didn’t necessarily remember this in the morning. Vasomotor disturbance (hot flushes) were correlated with poor scores on memory too. Their study found an average of 19 hot flushes a day. No wonder women are at their wit’s end! Sleep disturbance like the other things listed here can be caused by other factors, so again consider this as part of the whole picture.
HEADACHES
Migraines and tension headaches are common, again due to the drop in oestrogen. You might have noticed this just before a period in the past when oestrogen is at its lowest in the menstrual cycle. This can become more severe during Perimenopause. Some women also report dizziness and fatigue.
WEIGHT AND BODY CHANGES
Because oestrogen promotes muscle mass, when oestrogen starts to decline we lose muscle mass, meaning also that our metabolism slows down. Many women notice a shift in the body area where they store fat, from the thighs and bottom area to the belly. Menopause increases the production of deep tissue belly fat, known as visceral fat which is different to subcutaneous fat which is found elsewhere in the body and is just below the surface of the skin. This deep tissue fat is closely linked to increased risk of cardiovascular disease, type 2 diabetes, high blood pressure, breathing problems and even breast cancer. This is even true if your BMI is healthy but you are carrying extra weight around your middle. It’s generally agreed that a combination of healthy Mediterranean diet plus building and sustaining muscle mass helps. Muscle requires more energy to sustain it plus balances insulin and increases metabolism so win win win! The more muscle we have, our body is fighting fat even when we’re not actively working out – get in, where’s my dumbbells?
You might have also noticed a change in your hair where it might seem thinner and drier. Skin changes are common and can include dryness or acne, hairs sprouting, fine lines appearing or a combination of these factors, making it hard to keep up with what skincare works. Lack of collagen can leave skin feeling lack lustre and there are a confusing array of products out there. It’s best to get some advice then experiment with what works for you. Like everything, I think, don’t fight it, accept it, stay healthy, work out any old way, just move somehow, buy clothes that suit your new shape and please please don’t beat yourself up or compare yourself to others or your past self.
STEREOTYPICAL SYMPTOMS BUT TRUE!
We’ve touched on hot flushes as these are the hallmark symptom but cold sweats are also common. This is because the brain’s thermostat, the hypothalamus, becomes dysregulated due to lack of oestrogen. Vaginal dryness and discomfort during sex can occur as we lose oestrogen which would normally maintain the vagina’s lubrication. Sex drive can be sluggish, and this can be for a variety of reasons including tiredness, bleeding and mood changes, plus the discomfort mentioned. There are things you can do to improve all of this and your sex drive can improve, so please reach out, see your GP and try to make yourself comfortable again and remember, it’s temporary so may improve on its own or even get better than before! This is the wonder of the human body.
This is by no means an exhaustive list. Because we have oestrogen receptors all over the body including the brain, fluctuations in hormone levels can pretty much effect any system in the body. So if you perceive that something is different and it’s persisting and it’s distressing, please don’t deal with it alone. Reach out to a friend, family member, doctor, or any other woman! There is help and you can make it much more bearable and even – believe it or not, thrive. Perimenopause will be an individual experience for each woman and it’s an opportunity to focus on caring for ourselves after what may have been years of caring for and investing in others at work or home. As there’s still so much life left to live after Perimenopause our focus needs to be on making our lives work for us, which might mean that a combination of things are needed to change how you are experiencing your body’s and brain’s changes . This might be part medication, part lifestyle change, part reorientation on your values, part yoga retreat, part personal training session, part round the world trip (I wish!) …. The best might yet be still to come.
Image by Frank McKenna
